
Our Office
8-10 Saddle River Road
Fair Lawn, NJ 07410
Existing Patients: (201) 797-8711
New Patients: (201) 479-0901
Visit Us Online
If a dental professional has recommended a root canal, there’s no reason to panic. Advances in instruments, anesthetics, and techniques have made modern root canal therapy a predictable, comfortable way to treat a tooth whose inner tissues are compromised. In many cases, root canal treatment relieves persistent pain, removes infection, and preserves the natural tooth so you can maintain full function and appearance.
At Stahl Dental Studio we prioritize gentle, precise care and clear communication. Our team uses contemporary technology to diagnose problems early and to perform treatment efficiently, helping patients protect their long-term oral health with confidence.
Keeping a natural tooth whenever possible is usually the best option. A tooth that remains in place continues to support chewing function, maintain the jawbone, and preserve the alignment of neighboring teeth. Root canal therapy removes the damaged or infected tissue inside a tooth while maintaining the remaining structure, allowing that tooth to be restored and used for many years.
Success rates for non-surgical root canal treatment are high when the tooth is properly diagnosed and restored. The procedure focuses on eliminating bacteria from the internal spaces of a tooth, sealing the canals to prevent reinfection, and preparing the tooth for a durable final restoration such as a crown. When completed correctly, this combination of treatment and restoration helps reduce the chance of future problems.
For many patients, choosing root canal therapy means avoiding extraction and the need for more extensive replacement options. Saving the natural tooth often results in fewer long-term interventions and a more natural-feeling result compared with replacing a missing tooth.

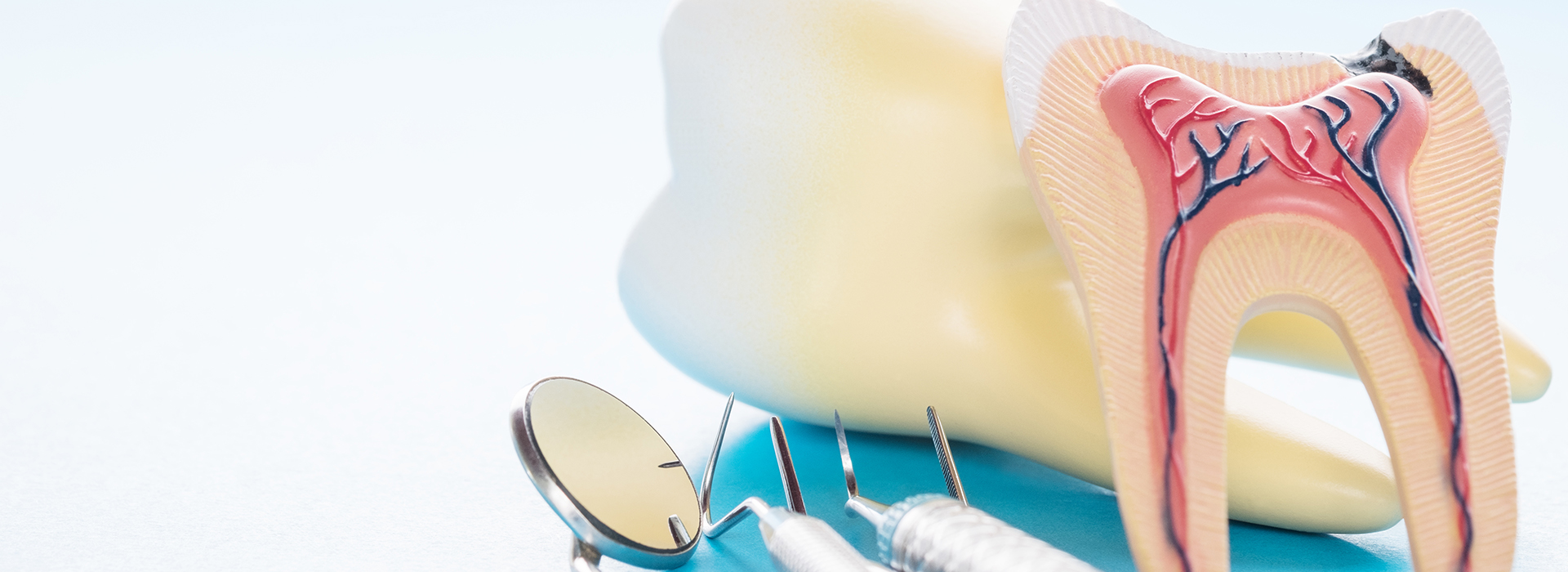
Teeth are more than the visible enamel and dentin; beneath those layers the dental pulp contains nerves, blood vessels, and connective tissue that keep the tooth vital during its development. When deep decay, a large restoration, repeated procedures, or trauma damages that internal tissue, inflammation or infection can develop and jeopardize the tooth’s health.
Symptoms that commonly accompany pulp damage include lingering sensitivity to hot or cold, sharp pain when biting, spontaneous throbbing discomfort, darkening of a tooth’s color, swelling in the gums near the affected tooth, or mobility if the supporting bone is compromised. Sometimes a tooth shows no obvious symptoms but reveals problems on a routine exam or an X-ray.
Not every ache means a root canal is required, but when the pulp is irreversibly inflamed or necrotic, root canal therapy is the standard approach to remove the diseased tissue and stop the spread of infection. Prompt assessment by a dental professional helps determine whether the internal tissues can be saved or whether treatment is necessary to prevent further complications.
Common warning signs that should prompt a prompt dental evaluation include:
Pain that lingers, intensifies with time, or disrupts sleep often indicates significant irritation or infection within a tooth. Early evaluation helps pinpoint the cause and outline appropriate treatment.
If hot or cold foods and beverages produce an extended or exaggerated reaction, the nerve tissues inside the tooth may be compromised and warrant examination.
Pain when applying pressure can signal that the internal tissues are inflamed or that an infection is affecting surrounding structures.
A tooth that becomes darker after an injury or over time can be a sign that internal tissues have changed or deteriorated.
Trauma that fractures tooth structure can also expose or damage the pulp, increasing the risk of infection and the need for root canal therapy.
Localized swelling, tenderness, or signs of an abscess indicate an active infection that requires timely professional care.
Inflammation and bone involvement related to an infected root can reduce support, producing mobility that often improves after appropriate treatment.

Addressing pulp problems early typically leads to simpler, more successful treatment and quicker recovery. When a tooth’s internal tissues are left untreated, infection can extend beyond the tooth into surrounding bone and soft tissues, increasing the complexity of care and potentially affecting adjacent teeth.
A routine dental exam or radiograph may reveal signs of root-end involvement or bone changes before you notice pain. That’s one reason regular checkups are important—so issues can be identified and managed before they escalate.
Delaying recommended treatment can result in more extensive care later. Acting promptly helps contain infection, preserve supporting structures, and often reduces the number of appointments needed to restore the tooth fully.
Root canal therapy today relies on precise instruments and materials that enable predictable cleaning, shaping, and sealing of the canals inside a tooth. Most treatments are performed under local anesthesia so you remain comfortable throughout the procedure. Additional anxiety-management options are available for patients who prefer them.
The process generally begins with isolating the tooth, creating a small access opening, and carefully removing the inflamed or infected pulp. The dentist then cleans and shapes the root canals, disinfects the internal spaces, and seals them with a biocompatible filling material to reduce the chance of reinfection.
Depending on the tooth’s anatomy and the presence of infection, a root canal can sometimes be completed in a single visit; other cases require more than one appointment to ensure thorough cleaning and healing. After the internal treatment is finished, the tooth is restored with a durable filling or crown to rebuild strength and protect the remaining structure.

Following a root canal, most patients experience a rapid reduction in the original tooth pain. Some tenderness or mild soreness around the treated tooth is common for a few days as the surrounding tissues heal. Over-the-counter analgesics are often sufficient, and more specific recommendations will be provided when needed.
It’s important to avoid chewing on the treated tooth until a permanent restoration is in place; teeth that have had root canals can be more prone to fracture until they are fully restored with a crown or similar solution. Maintaining good oral hygiene and attending follow-up visits helps protect the treated tooth and the health of the entire mouth.
If you notice persistent swelling, a return of pain, spreading redness, or any other concerning signs after treatment, seek prompt evaluation so any problems can be addressed quickly. With proper care, a root canal–treated tooth can remain functional for many years, often for the remainder of a patient’s life.
At Stahl Dental Studio, our approach combines careful diagnosis, modern techniques, and clear patient education so you can make informed decisions about preserving your smile. If you would like to learn more about root canal therapy or schedule an appointment, please contact our office for additional information.
A root canal is a dental procedure that removes diseased or damaged tissue from inside a tooth to preserve the remaining structure. The treatment targets the dental pulp, the soft tissue containing nerves, blood vessels and connective tissue that occupies the tooth’s central chamber. By eliminating infection and sealing the canals, a root canal restores the tooth’s health and function while avoiding extraction.
Root canal therapy is a standard endodontic treatment performed with modern instruments and materials designed to clean and shape the internal canals. After the canals are cleaned and filled with a biocompatible material, the tooth is typically restored with a durable restoration to protect it from fracture. When performed correctly, the procedure preserves natural dentition and supports long-term oral health.
You may need a root canal when the dental pulp becomes inflamed, infected or has died due to deep decay, traumatic injury or repeated dental procedures. When pulp tissue is compromised, bacteria can spread through the root system and cause pain, swelling or radiographic evidence of periapical pathology at the root tip. Timely root canal therapy removes the source of infection and prevents further damage to surrounding tissues.
Left untreated, an infected tooth can lead to worsening pain, bone loss around the root and systemic health concerns in some cases. A comprehensive dental exam and radiographs help confirm whether pulp involvement requires root canal treatment. Early evaluation improves the likelihood of saving the natural tooth and minimizing complications.
Common warning signs include persistent or severe tooth pain, especially pain that wakes you at night, and heightened sensitivity to hot or cold that lingers after the stimulus is removed. You may also experience tenderness when biting or chewing, swelling of the gums near the affected tooth, or a visible darkening or discoloration of the tooth. These symptoms often indicate that the inner pulp is inflamed or infected and warrants prompt evaluation.
Some teeth with pulp damage can be asymptomatic and are discovered during routine exams or on dental X-rays when radiographic signs of root-end pathology are present. Other indicators include a loose tooth or a draining gum tract near the tooth, which suggest an advancing infection. Because symptoms vary, a dental professional should evaluate any persistent oral changes to determine the appropriate care.
Root canal therapy begins with administering local anesthesia to ensure the procedure is comfortable and pain-free. The dentist creates a small opening in the crown to access the pulp chamber, then carefully removes diseased tissue and shapes the internal canals with specialized instruments. The canals are irrigated to eliminate bacteria and disinfect the space before being filled with a biocompatible material to seal the canals.
After the internal portion of the tooth is treated, a temporary filling is commonly placed and the tooth is evaluated for a definitive restoration such as a crown. Some cases are completed in a single visit while others require multiple appointments depending on anatomy, the number of canals and whether active infection is present. Final restoration is important to restore strength and prevent future fracture or reinfection.
Modern root canal procedures are typically no more uncomfortable than receiving a routine dental filling thanks to effective local anesthesia and gentle techniques. Many patients report that the pain prompting the visit is more significant than the procedure itself, and anesthesia ensures the treatment is well tolerated. For patients with dental anxiety, sedation options are available to enhance comfort and reduce stress during care.
It is common to experience mild to moderate soreness for a few days after the procedure as surrounding tissues heal, and over-the-counter analgesics or prescribed medications can manage this discomfort. Persistent or severe pain, swelling or signs of infection after treatment should be evaluated promptly by your dentist to determine whether additional care is needed. Communication with your dental team ensures appropriate follow-up and relief.
Immediately after treatment you may have lingering numbness for an hour or two and should avoid chewing until a permanent restoration is placed to prevent accidental injury. Mild tenderness or sensitivity is normal for a few days as the tissues recover, and your dentist may adjust the bite to minimize pressure on the treated tooth. If antibiotics or pain medication are prescribed, follow the instructions carefully and complete the antibiotic course if directed.
Good oral hygiene — brushing twice daily, daily flossing and regular dental checkups — supports healing and long-term success of the treated tooth. Because a tooth that has undergone root canal therapy can be more prone to fracture, timely placement of a permanent crown or appropriate restoration is important to restore strength and function. Report any new symptoms, persistent discomfort or changes in the treated tooth to your dental provider for evaluation.
Root canal therapy has a documented success rate that is generally high when performed and restored properly, and many treated teeth function for years or a lifetime. Potential risks include persistent or recurrent infection, canal anatomy that is difficult to fully clean, post-treatment fracture of the tooth and the occasional need for retreatment or surgical endodontic procedures. These risks vary with the extent of initial damage, the tooth’s anatomy and how promptly the tooth is restored after treatment.
Close follow-up, appropriate restoration and good oral hygiene help reduce the likelihood of complications and improve long-term outcomes. If symptoms recur, additional imaging and evaluation can determine whether retreatment, endodontic surgery or other interventions are indicated. Discussing specific risks and prognosis with your dentist provides clarity based on your individual case.
The primary alternative to root canal therapy is extraction of the affected tooth followed by a replacement option such as a dental implant, bridge or removable prosthesis. Each alternative has clinical considerations: extraction eliminates the infected tissue but also removes the natural tooth, and replacement options differ in terms of surgical requirements, restorative planning and long-term maintenance. Preservation of the natural tooth with root canal therapy is often preferred when feasible because it maintains natural chewing function and bone support.
Determining the best approach involves evaluating the tooth’s restorability, surrounding bone support and overall oral health. Your dentist can review the clinical findings, radiographs and restorative needs to recommend the most appropriate treatment path. Shared decision-making ensures the chosen option aligns with your oral health goals and clinical circumstances.
With proper care and a well-sealed restoration, a tooth treated with root canal therapy can last for many years and in many cases a lifetime. Longevity depends on factors such as the quality of the root canal filling, the fit and strength of the final crown or restoration, the amount of remaining tooth structure and your ongoing oral hygiene habits. Regular dental examinations and radiographs help detect changes early so interventions can protect the treated tooth.
Occasionally a treated tooth may require retreatment or additional procedures if new decay, a breakdown of the restoration or an anatomical complication arises. Prompt attention to new symptoms, routine professional care and avoiding excessive forces on the treated tooth all contribute to long-term success. Your dentist will advise on maintenance and monitoring tailored to your situation.
At Stahl Dental Studio our approach to root canal care emphasizes accurate diagnosis, effective infection control and careful restoration to protect the long-term health of the tooth. We use contemporary endodontic techniques and infection-control protocols to clean and seal canals precisely, and we coordinate subsequent restorative treatment to restore function and strength. Patient comfort and clear communication about the procedure and follow-up care are integral to the treatment process.
The decision to preserve a tooth with root canal therapy is based on clinical evaluation, radiographic findings and restorative considerations unique to each patient. When additional support or specialty care is helpful, we collaborate with endodontic or restorative specialists to achieve the best possible outcome. If you have symptoms or concerns about a tooth, scheduling an evaluation allows the team to recommend the appropriate next steps.
